Artificial Intelligence (AI) is revolutionizing healthcare, and its impact on amputee care is nothing short of transformative. These innovations are not only improving mobility and functionality but also enhancing quality of life and independence. Read here how AI is paving the way for smarter, more intuitive solutions in amputee care. Questions? We are here to answer them!
Some would argue that artificial intelligence has been improving amputees’ lives since the 1960s, with the introduction of pattern recognition in myoelectric arms. At the very latest, AI-driven prosthetic technology has been around since the 1990s, when the C-Leg debuted. And almost all would agree that there’s enormous potential for future growth in this realm (viz. “The Midas Touch” in our new print edition).
But the emergence of ChatGPT and other large-language models (LLMs) has vastly broadened the potential for amputee-serving AI applications. In addition to making prosthetic limbs more lifelike than ever, AI is now driving innovation in socket design, prosthesis alignment, adaptive fitness, caregiving, and beyond.
We surveyed the literature to get a sense of where and how researchers are employing AI to enhance (and potentially transform) limb care. Not all of these applications are in clinical use yet, and some may never get there. But one way or the other, the algorithms are on the march and there’s no stopping them. Here’s how AI might impact your life before long.
Supporting caregivers: Researchers at the University of Pittsburgh developed a responsive knowledge base called CaLM (Caregiver Language Model). The prototype, aimed at caregivers of patients with Alzheimers and related forms of dementia, allows users to get accurate, real-time information to answer their questions and ease their anxieties. “The intricate care requirements associated with [cognitive and behavioral diseases] present a complex challenge that caregivers must navigate, often without formal training,” the authors write. “Given the progressive nature of these conditions, caregivers are in need of long-term support and strategies, underlining the importance of a dedicated resource like the CaLM….The model can provide substantial support to a vast community of caregivers who are frequently underserved when it comes to specialized care resources.” The researchers hope to expand on this pilot project to develop parallel tools for other conditions requiring ongoing care, including limb loss. Read the full paper at JMIR Formative Research.
Streamlining socket fabrication: Members of an international collective called the Residual Limb Shape Capture Group introduced a novel approach using AI to develop digital socket templates based on a prosthetist’s previous work in traditional (plaster-based) fabrication. Using 3D scans, the AI essentially learns a given prosthetist’s methods for manual fabrication, then translates that knowledge into templates for new limb models. “The AI-generated sockets closely matched those made by hand, with only small differences,” the authors conclude. “This new process has the potential to save time and make socket fitting more consistent, helping individuals with amputations receive faster and more accurate prosthetic care.” Here’s the full paper at Prosthesis.
Managing exercise: A pair of experts in diabetes management and rehabilitation found the subscription-only version of ChatGPT to be a reliable source of information about exercise for Type 2 diabetes patients. They asked ChatGPT for the best clinical recommendations about exercise types, frequency, intensity, duration, etc., along with questions related to nutrition, weight maintenance, comorbidities (such as kidney disease), and other aspects of fitness. “ChatGPT provided relatively valid, safe and useful information about exercise for type 2 diabetes,” the authors concluded, but they added a couple of caveats: Patients should only use ChatGPT in conjunction with medical guidance from a human clinician, not as a primary source of information; and the finding doesn’t apply to the free version of ChatGPT (currently v4o). Read the full paper at BMJ Health & Care Informatics.
Standardizing prosthesis alignment: After a systematic literature review, a team of biomechanics experts concluded that AI algorithms and alignment tools hold tremendous potential to enhance accuracy and reduce human error in transtibial prosthesis alignment. “Current practices for transtibial prosthesis alignment lack standardization, leading to various health complications,” the authors assert. “The absence of automated approaches for prosthesis alignment hinders the accuracy and efficiency of the alignment process.” The need is particularly acute in developing nations where the availability of clinical expertise falls far short of the demand. The full paper is paywalled, but you can read the abstract and introduction at Artificial Intelligence in Medicine.
Determining amputation level: This one scares us a little….okay, a lot. Orthopedists at the Ege University School of Medicine in Izmir, Turkey, submitted clinical photographs of diabetic foot ulcers to ChatGPT and asked it to recommend the optimal amputation level. In 50 out of 60 cases, the bot’s recommendation was identical to the amputation the human clinicians actually performed. In the remaining 10 cases, ChatGPT prescribed a more proximal (ie, higher) amputation than the flesh-n-blood docs. “Relying solely on clinical photographs,” the paper concluded, “ChatGPT-4.0 demonstrates decisions that are largely consistent with those of an experienced team in determining the optimal level of amputation for DFUs.” Personally, we’re a long way from trusting ChatGPT to dictate a surgical procedure; we don’t even trust it to write email for us. But read the abstract at the International Wound Journal and judge for yourself (full paper is paywalled).
Optimizing MPK leg controllers: Here’s where things start to get meta. Levi Hargrove and colleagues at the Shirley Ryan AbilityLab are working on a process in which AI-generated gait patterns are used to improve the performance of a bionic leg’s mid-level controller—which is itself an AI-equipped unit. In other words, it’s an AI trainer for an AI device. Crazy, right? The core benefit of such a system would be to eliminate the need to gather training data from individual volunteers, which would a) make the training of prosthetic leg controllers more efficient and more effective, and b) lower R&D costs and (in theory, anyway) accelerate the pace of innovation. The system’s still in development and hasn’t been tested with actual prosthesis users yet, but it doesn’t pay to bet against Hargrove. Full study at the Journal of Neuroengineering and Rehabilitation.
Assessing limb-loss risk in PAD patients: A Mayo Clinic team trained AI to analyze Doppler waveforms in patients with peripheral artery disease and accurately assess the risk of limb loss. In a study encompassing more than 2,000 patients over a five-year period, the AI tool accurately predicted adverse outcomes including death, major cardiac events, and limb loss. “The AI tool described in this article has several unique advantages whereby both the 1‐ and 5‐year risk for [limb loss] can be estimated well before chronic limb‐threatening ischemia occurs, solely on the basis of deep neural assessment of a posterior tibial arterial waveform Doppler signal,” the authors explain. By combining AI analysis with an easy‐to‐perform, noninvasive Doppler test, clinicians can better identify at-risk patients before their symptoms become acute and intervene early enough to prevent some amputations. Read it all at the Journal of the American Heart Association.
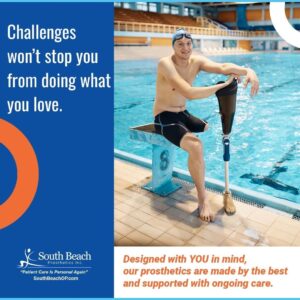
Promoting participation in parasports: A Brazilian bioscientist is exploring AI’s potential to help people with disabilities overcome barriers to participation in physical fitness activity. “Personal and environmental obstacles linked to disability hinder access to venues and services,” he observes. Many amputees are deterred from exercise by the logistical complexities of acquiring equipment, traveling to fitness facilities, and receiving informed coaching. Once they’ve solved those problems, amputees must still overcome factors such as pain, stamina, and discomfort about exercising in public settings. “AI has now emerged as a promising tool to overcome these barriers, offering innovative and personalized solutions to meet the individual needs of those who use it,” the paper concludes. It’s paywalled at the Journal of Bodywork and Movement Therapies.
Experience the latest in prosthetic technology with our advanced prosthetic solutions. Our expert team will work closely with you to find the best solution for your unique needs and help you get back to living life to the fullest. Contact us today at 888-819-4721. Follow us on Instagram for more tips.
Reference: [https://livingwithamplitude.com/ai-amputee-care-artificial-intelligence/]